Data can easily be manipulated if it is not complete and reported in a rational and honest manner.
Original article dated APRIL 21, 2021.
After using the same data interpretation policy for 17 years, the CDC in March 2020 suddenly made a quantum change in the way data was interpreted and reported.
And it turns out… this is a serious breach of US Federal Law.
Why would the CDC decide against using a system of data collection & reporting they authored, and which has been in use nationwide for 17 years without incident, in favor of an untested & unproven system exclusively for COVID-19 without discussion and peer-review?
The “Institute for Pure and Applied Knowledge (IPAK)” has completed and investigation as to exactly what happened and it is very alarming.
To understand the significant implications of these guidelines and how they substantially emphasized COVID-19 as a cause of death, while simultaneously deemphasizing comorbidity (pre-existing conditions) in cause of death records.
Despite the CDC’s March 9, 2020 admission that the highest risk group of Americans would be over 60 years of age and have pre-existing conditions, only 7 state health departments are reporting comorbidity in a manner that can be statistically analyzed (New York Pennsylvania, Massachusetts, Georgia, Utah, Oklahoma, Iowa).
Would the 94% of fatalities with at least 1 comorbidity have been counted as COVID-19 fatalities if the CDC had used the guidelines for reporting they had used for the past 17 years instead of the COVID-19 guidelines issued on March 24, 2020?
Spoiler Alert, no they would not have been counted.
To properly answer this question, it is necessary to compare the unproven March 24 COVID- 19 Alert No. 2 cause of death reporting guidelines against the 2003 CDC Medical Examiner’s and Coroner’s Handbook on Death Registration that has been the proven national standard for 17 years without incident.
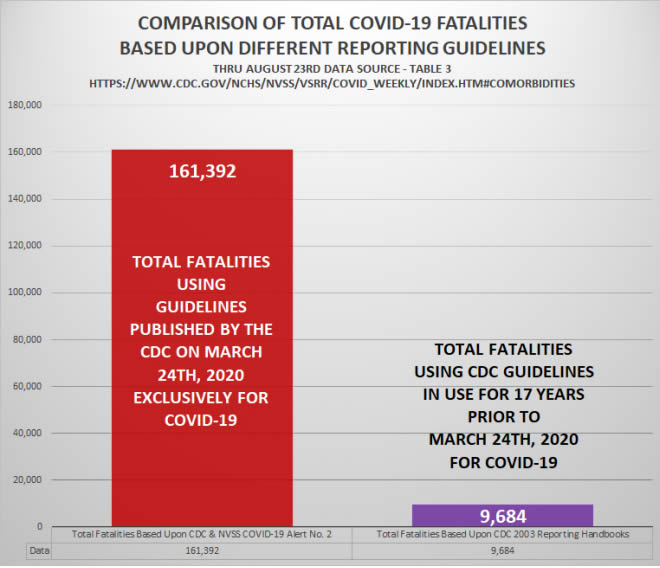
ABOVE: Using the NEW March 24, 2020 Data Guidelines vs Using the 2003 Guidelines that were in place for 17 years.
Had the CDC used the 2003 guidelines, the total COVID-19 be approximately 16.7 times lower than is currently being reported
Comorbid conditions have been listed on Part I of death certificates as causes of death per the CDC Handbook since 2003 to ensure accurate reporting can be developed. Comorbidities are seldom placed in Part II. Part II is typically the section where coroners and medical examiners can list recent infections as underlying, initiating factors.
Prior to the CDC’s March 24th policy change, any comorbidities would have been listed in Part I rather than Part II and initiating factors such as infections including the SARS-COV-2 virus, would have been listed on the last line in Part I or more commonly in Part II.
Under these 2003 guidelines, the highest COVID-19 could be listed in the presence of an established comorbidity would be on the lowest used line at the bottom of Part I as an initiating factor or, more correctly, in Part II as an infection that contributed to death.
However, on March 24, 2020 the CDC elected to forgo this trusted method of cause of death recording in favor of recording comorbidities in Part 2, so COVID-19 could be listed exclusively in Part 1.
This has had a significant impact on data collection accuracy and integrity. It has resulted in the potential false inflation of COVID-19 fatality data and is a potential breach of federal laws governing information quality.
CDC COVID-19 Alert No. 2 guidelines published by the CDC and the revelation presented at the beginning of this historical retrospective, “For 6% of the deaths, COVID-19 was the only cause mentioned. For deaths with conditions or causes in addition to COVID-19, on average, there were 2.6 additional conditions or causes per death.”
Federal agencies have a legal obligation to provide the most accurate data to the public, fellow agencies, and policy makers they are advising, and they have a responsibility to abide by every federal law. This responsibility to collect, analyze, and publish data accurately, transparently, and with unquestionable integrity increases exponentially during a national crisis.
It is concerning that the CDC may have willfully failed to collect, analyze, and publish accurate data used by elected officials to develop public health policy for a nation in crisis.
Further federal investigation is justified by the magnitude of the crisis and the collateral damage generated by policies based upon projection data that was unproven and never peer reviewed. If the data being reported was indeed compromised by the CDC’s perplexing decision to abandon proven data collection and reporting practices in favor of untested methods, then all public health policies based upon these inaccurate data must be reexamined.
Download the Institute for Pure and Applied Knowledge (IPAK) REPORT here: USA COVID data collection 2021 REPORT
THE SECOND CDC POLICY CHANGE
Another quantum change the CDC did was change the rules on determining a COVID death on death certificates.
“They now instruct doctors that they can assume a covid death without any testing.”
See the CDC directive for yourself on the CDC website here:
https://www.cdc.gov/nchs/data/nvss/coronavirus/Alert-1-Guidance-for-Certifying-COVID-19-Deaths.pdf
This has never been the standard of reporting for any cause of death until April 2020. Watch these government health officials explain what is called a “covid death”.
Watch Doctor Jensen explain what the change was and how it impacts the data that we are seeing.
DO HOSPITALS GET PAID MORE MONEY FOR A COVID-19 DEATH?
Lets see what the mainstream media has found…
ABC News
“HHS reported, 63 California hospitals, received $50,000 for each eligible coronavirus patient they admitted between Jan. 1 and June 10, 2020. That’s a combined total of more than $607 million.”
USA Today
USA Today did a Fact Check article on this point and also found it to be TRUE.
“We rate the claim that hospitals get paid more if patients are listed as COVID-19 and on ventilators as TRUE.”
“Hospitals and doctors do get paid more for Medicare patients diagnosed with COVID-19 or if it’s considered presumed they have COVID-19 absent a laboratory-confirmed test, and three times more if the patients are placed on a ventilator to cover the cost of care and loss of business resulting from a shift in focus to treat COVID-19 cases.”
USA Today Fact Check article link: https://www.usatoday.com/story/news/factcheck/2020/04/24/fact-check-medicare-hospitals-paid-more-covid-19-patients-coronavirus/3000638001/
Los Angeles Times
Los Angeles Times found that Nursing homes could be paid four times more for coronavirus patients than for other residents and that Coronavirus patients could be cash cows for nursing homes.
“COVID-19 patients can bring in upward of $800 per day, according to nursing home administrators and medical directors interviewed by The Times.
By contrast, facilities collect as little as $200 per day for long-term patients with dementia.”
Los Angeles Times article: https://www.latimes.com/california/story/2020-05-03/coronavirus-nursing-homes-financial-profits
Washington Examiner
Washington Examiner reported CDC director acknowledges hospitals have a monetary incentive to over count coronavirus deaths.
U.S. Centers for Disease Control and Prevention Director Robert Redfield agreed that some hospitals have a monetary incentive to over count coronavirus deaths as they do deaths for other diseases.
“I think you’re correct in that we’ve seen this in other disease outbreaks too. Really, in the HIV epidemic, somebody may have a heart attack but also have HIV — the hospital would prefer the classification for HIV because there’s greater reimbursement,” Redfield said during a House panel hearing Friday when asked by Rep. Blaine Luetkemeyer about potential “perverse incentives.”




Leave a Reply
You must be logged in to post a comment.